Azoospermia, the absence of sperm in semen, is a significant cause of male infertility. Diagnosing azoospermia is the first step toward understanding its underlying causes and exploring potential treatment options. One of the primary diagnostic tools for detecting azoospermia is a semen analysis normal report. This non-invasive and detailed test evaluates various aspects of male reproductive health, including the presence or absence of sperm.
What Is Azoospermia?
Azoospermia is a condition where no sperm are found in the ejaculate. It can be classified into three main types:
- Pre-testicular Azoospermia: Caused by hormonal imbalances or genetic conditions that impair sperm production.
- Testicular Azoospermia: Results from damage or abnormalities in the testes.
- Post-testicular Azoospermia: Occurs when sperm production is normal, but an obstruction in the reproductive tract prevents sperm from appearing in the semen.
Identifying the type of azoospermia is crucial for determining treatment options.
The Role of Semen Analysis in Diagnosing Azoospermia
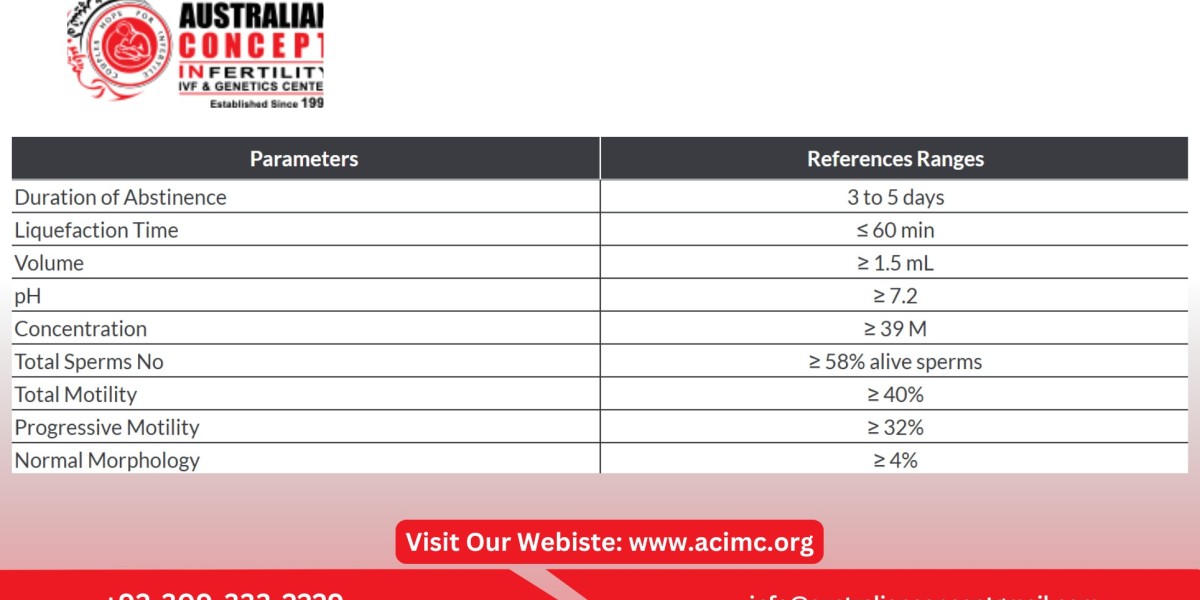
Semen analysis is a comprehensive test that evaluates the quality and quantity of sperm. Here’s how it helps in diagnosing azoospermia:
1. Absence of Sperm in Semen
During the test, a laboratory technician examines the semen sample under a microscope. In cases of azoospermia, no sperm will be detected even after an extended search.
2. Volume and Appearance of Semen
Semen volume and viscosity can indicate potential issues. Low volume may point to ejaculatory duct obstruction or retrograde ejaculation.
3. pH Levels
Abnormal pH levels in the semen may suggest an obstruction in the reproductive tract, commonly associated with post-testicular azoospermia.
4. White Blood Cells and Other Components
The presence of white blood cells in semen might indicate infection or inflammation, which can sometimes mimic azoospermia.
Confirmatory Tests Following Semen Analysis
If azoospermia is suspected based on semen analysis, additional tests are usually recommended to confirm the diagnosis and pinpoint the cause:
1. Hormonal Testing
Blood tests measure hormone levels such as FSH, LH, and testosterone. Elevated FSH levels might indicate testicular azoospermia, while low levels could suggest hormonal imbalances.
2. Ultrasound Imaging
Scrotal or transrectal ultrasound can help detect blockages, cysts, or other abnormalities in the reproductive tract.
3. Genetic Testing
Genetic evaluations may identify conditions like Klinefelter syndrome or Y-chromosome microdeletions, which are linked to azoospermia.
4. Testicular Biopsy
A small tissue sample from the testes is examined to determine if sperm production is occurring. This test is often used when hormonal levels and semen analysis results are inconclusive.
Why Early Diagnosis Matters
Diagnosing azoospermia early is essential for exploring potential treatments and fertility options. Depending on the type and cause of azoospermia, treatments may include:
- Surgical Interventions: To remove blockages in the reproductive tract.
- Hormonal Therapy: For cases related to hormonal imbalances.
- Assisted Reproductive Techniques (ARTs): Sperm retrieval methods like testicular sperm extraction (TESE) can be combined with ICSI treatment to enable conception.
Conclusion:
A semen analysis normal report is a crucial diagnostic tool for detecting azoospermia, providing detailed insights into sperm presence and semen characteristics. If azoospermia is identified, further tests help determine its type and underlying causes, paving the way for targeted treatments. Early diagnosis and consultation with an infertility specialist can significantly improve the chances of overcoming this condition and achieving parenthood.